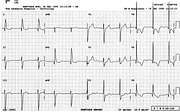
Atypical LBBB: Anterolateral Q Waves
Report:
Sinus rhythm
SVEBs, runs of SVT
Left axis deviation –50o
Intraventricular conduction delay, probably atypical left bundle branch block
Probable old anterior infarction
ST/T changes suggest infarction/ischæmia.
Comment:
Post-arrest ECGs (and enzymes) are often difficult to interpret; fortunately it does not really matter that much whether the patient had actual infarction or only ischaemia. His future depends on his coronary anatomy.
The following day the ST segments resumed their usual position (below, Fig 48a), similar to that of pre-admission traces (not shown).
The QRS delay is all in the left ventricular territory, but the Q waves make the diagnosis of LBBB difficult. They indicate anteroseptal infarction in LBBB, although many patients with LBBB and anteroseptal infarct do not have them. IVCD is a safe diagnosis. John Morgan, Director of Cardiology at St. Vincent’s Hospital in Sydney, gave me this excellent advice when I asked him how to report ECGs: “Under-report them!”.
If you have any suggestions for or feedback on this report, please let us know.
Hi, can we chat about some terms and conditions?
The library and it's records are licensed under the Creative Commons Attribution 4.0 International license.
You are free to:
- Share — copy and redistribute the material in any medium or format for any purpose, even commercially.
- Adapt — remix, transform, and build upon the material for any purpose, even commercially.
- The licensor cannot revoke these freedoms as long as you follow the license terms.
Under the following terms:
- Attribution — You must give appropriate credit , provide a link to the license, and indicate if changes were made . You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
- No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
By clicking agree below, you are agreeing to adhere to CC BY 4.0.