Right Ventricular Pulmonary Œdema
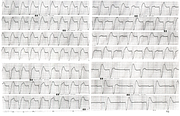
Report:
Sinus tachycardia
Right axis deviation +95o
Incomplete RBBB
Clockwise rotation
Non-specific ST/T changes, consistent with ischæmia
Comment:
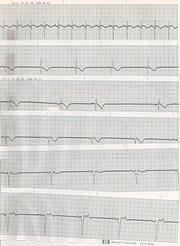
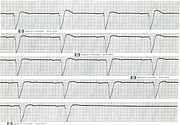
The repolarisation changes probably reflect the patient’s gross hypoxia on admission. The ECG evolved along the usual “RV strain” morphologies (next page, Fig 203a), with RAA and right precordial T wave inversion; it normalised within three months. His chest X-ray is shown in Fig 203b.
The pulmonary œdema fluid on admission had low albumin content of a transudate, despite low wedge pressure; this rose to high levels seen in ARDS within 24 hours. The most likely mechanism of the initial œdema was transudation from overperfusion and massive pulmonary hypertension generated by the right ventricle! To my knowledge, no analogous cases have been documented as yet146.
This patient had three admissions to ICU, all three with pulmonary œdema in the “good” lung. I intubated him three times and treated him, more or less expectantly, with antibiotics and thrombolytics and heparin, thinking of what could have raised the pulmonary pressures. First two times were a great success and I thought I was very clever (I diagnosed the hypoplasia after reading a NEJM article on high-altitude pulmonary oedema147). Hubris: third time he had a cerebral hæmorrhage and died. Now I still feel the guilt. Primum non nocere and all that.
Autopsy confirmed the angiography findings. There was severe left and mild right upper lobe pulmonary artery hypoplasia with small-diameter but normal aorta. And the cerebral bleed.
His Ventilation-perfusion scans (Figs 203b, 203c) and pulmonary angiogram (Fig 203d) are shown below.
If you have any suggestions for or feedback on this report, please let us know.
Hi, can we chat about some terms and conditions?
The library and it's records are licensed under the Creative Commons Attribution 4.0 International license.
You are free to:
- Share — copy and redistribute the material in any medium or format for any purpose, even commercially.
- Adapt — remix, transform, and build upon the material for any purpose, even commercially.
- The licensor cannot revoke these freedoms as long as you follow the license terms.
Under the following terms:
- Attribution — You must give appropriate credit , provide a link to the license, and indicate if changes were made . You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
- No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
By clicking agree below, you are agreeing to adhere to CC BY 4.0.