Hypokalæmia
Report:
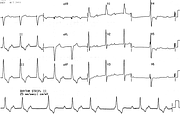
Sinus rhythm.
Borderline left axis deviation -30o.
Prominent repolarisation changes suggestive of hypokalæmia.
Comment:
The patient had severe metabolic acidosis and marked, paralysing hypokalæmia (K 1.7 mEq/L) No cause was found during her 4-day long stay in the ICU, but, some weeks later, renal tubular acidosis due to Sjogren’s syndrome was diagnosed.
The U waves are so large that they may be mistaken for T waves. The U waves became more discrete in the tracing below (Fig 264a), at K 2.0 mEq/L. They stand up for themselves quite well in V2-3. Eventually (not shown) her ECG became normal
Hyperthyroid Hypercalcæmia on Lithium Therapy
Report:
Sinus tachycardia 163/min
Borderline right atrial abnormality
Borderline short QT interval 0.22”
Nonspecific T wave changes
Comment:
Marked tachycardia with short QT interval gives an illusion of atrial flutter. Indeed, the patient was treated with digoxin and amiodarone for flutter, without success! She was also given lithium carbonate, as the serum level was subtherapeutic (0.2); the level rose to mildly toxic range (1.4). Serum calcium was 3.8 mmol/L! She became obtunded and hypercarbic and was transferred to ICU, where therapy was repeatedly delayed by (of all people) her Endocrinologist197!
Thyroid hormones were grossly elevated: T4 76 [8-22], T3 4.3 [1-2.4], with suppressed TSH 0.04 [0.17-2.9]. Thus she had two reasons for hypercalcæmia: hyperthyroidism and lithium therapy198. She had three reasons for obtundation: hypercalcæmia, thyroid storm itself, and the lithium toxicity.
The QT interval is often difficult to measure. The QTc obtained for the rate 163/min and QT 0.22” was 0.40” (normal) by one method and 0.367” (minimally shortened) by another (Bazett’s).
QTc = QT + 1.75(rate-60) = 400.25 msec
QTc = QT/Square root RR = 0.367 sec
ECG is not a very useful tool in this setting, although it was virtually diagnostic of thyrotoxicosis in the setting of unexplained, striking sinus tachycardia. The QRS complex is probably mildly prolonged, increasing the measured QT interval; the PR interval is similarly prolonged, making the T-P junction the end of T wave in most leads; in addition, large variety of factors may be actually prolonging the QT interval in a sick elderly patient. One such factor is thyrotoxicosis itself199.
The RAA may be spurious, since hyperthyroidism increases all ECG voltages (opposite of better known reduction of ECG amplitude in myxœdema). At least in part, increased P wave amplitude is due to tachycardia itself.
If you have any suggestions for or feedback on this report, please let us know.
Hi, can we chat about some terms and conditions?
The library and it's records are licensed under the Creative Commons Attribution 4.0 International license.
You are free to:
- Share — copy and redistribute the material in any medium or format for any purpose, even commercially.
- Adapt — remix, transform, and build upon the material for any purpose, even commercially.
- The licensor cannot revoke these freedoms as long as you follow the license terms.
Under the following terms:
- Attribution — You must give appropriate credit , provide a link to the license, and indicate if changes were made . You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
- No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
By clicking agree below, you are agreeing to adhere to CC BY 4.0.